read this about heat and transdermal aplication...below...
Expert Opin Drug Deliv. Author manuscript; available in PMC 2017 May 1.
Published in final edited form as:
Expert Opin Drug Deliv. 2016 May; 13(5): 755–768.
Published online 2016 Jan 25. doi: 10.1517/17425247.2016.1136286
PMCID: PMC4841791
NIHMSID: NIHMS771879
PMID: 26808472
Heat effects on drug delivery across human skin
Jinsong Hao,a Priyanka Ghosh,b S. Kevin Li,c Bryan Newman,b Gerald B. Kasting,c and Sam G. Raneyb
Author information Copyright and License information Disclaimer
The publisher's final edited version of this article is available at Expert Opin Drug Deliv
See other articles in PMC that cite the published article.
Go to:
Abstract
Introduction
Exposure to heat can impact the clinical efficacy and/or safety of transdermal and topical drug products. Understanding these heat effects and designing meaningful in vitro and in vivo methods to study them are of significant value to the development and evaluation of drug products dosed to the skin.
Areas covered
This review provides an overview of the underlying mechanisms and the observed effects of heat on the skin and on transdermal/topical drug delivery, thermoregulation and heat tolerability. The designs of several in vitro and in vivo heat effect studies and their results are reviewed.
Expert opinion
There is substantial evidence that elevated temperature can increase transdermal/topical drug delivery. However, in vitro and in vivo methods reported in the literature to study heat effects of transdermal/topical drug products have utilized inconsistent study conditions, and in vitro models require better characterization. Appropriate study designs and controls remain to be identified, and further research is warranted to evaluate in vitro-in vivo correlations and the ability of in vitro models to predict in vivo effects. The physicochemical and pharmacological properties of the drug(s) and the drug product, as well as dermal clearance and heat gradients may require careful consideration.
Keywords: dermal clearance, heat effect, heat exposure, patch, skin blood flow, topical drug products, transdermal delivery systems (TDS)
Go to:
1. Introduction
Drug products administered via the skin are typically classified as being either topical or transdermal drug products. When the intended site of action for drugs dosed to the skin is the skin itself, the route of administration is considered to be topical (local). When the intended site of action is systemic, the route of administration is considered to be transdermal. This review focuses on topical and transdermal drug delivery systems that are designed to deliver drugs into and/or through the skin at a relatively controlled rate for a specified duration. The most common are the drug-in-adhesive-matrix-based products, which are classified as extended release film dosage forms, with which the drug is classified to be dosed by a transdermal route of administration. Compendial references often refer to these as transdermal delivery systems (TDS), although TDS can also include reservoir-based drug products or active iontophoretic delivery systems. Less common are topical patch delivery systems, which are indicated for local as opposed to systemic effect; for these products, the drugs are classified to be dosed by a topical route of administration, and the dosage form is classified as a patch. While we predominantly focus on TDS in this review, some of the issues may apply equally to topical patches.
An increasing body of evidence indicates that elevated temperature during the normal course of product wear can substantially disrupt the well-controlled, steady drug delivery rate that is characteristic of TDS. TDS deliver drugs across the stratum corneum (SC) barrier and viable epidermis into the dermis, from which the drug can be cleared by the dermal capillaries. Local or systemic exposure to heat can change the drug release from the TDS, as well as the barrier properties of the SC and/or the rate of dermal clearance, thereby collectively altering drug delivery. The effects of heat from hot showers or baths, saunas, electric blankets and other such heat sources on these dosage forms are of interest to characterize because in order to sustain a nominal drug delivery rate over a prolonged period, TDS routinely contain an excess drug load that is not intended to be delivered to the patient. In situations where the rate and extent of drug delivery are increased by heat exposure, the excess drug load can dose the patient substantially above approved levels. As such, heat effects with TDS dosage forms are critically important because these effects may result in an altered rate profile for dosing, along with a substantially increased total dose and an altered safety profile. Furthermore, since TDS deliver drugs into the systemic circulation, the increase in delivery rate and amount dosed could have significant, unintended systemic effects.
The effects of heat (i.e. elevated temperature) on TDS can vary in severity, depending on the formulation and/ or the design of the TDS; the effect of heat on certain drug products like fentanyl TDS could even be fatal.[1–4] A sufficient body of evidence now exists to support the need for a more comprehensive understanding of the effects of heat on the potential safety and effectiveness of TDS. This review will provide an overview of the effects of heat on factors that influence transdermal and topical drug delivery, including drug release from the TDS, drug partitioning into the SC, drug diffusion within the skin, and dermal clearance of the drug from the application site. The distinct effects of elevated temperature on the product formulation, on the release of drug from the delivery system, on the skin, and on the permeation of the drug through the skin have not been adequately characterized in the existing literature and may be difficult to deconvolute. In addition to the discussion of physiological factors related to thermal stress and their impact on dermal clearance, the emphasis in the present review will be given to reviewing the published studies demonstrating the impact of elevated temperature on drug release and skin permeation in vitro and in vivo from topical delivery systems and TDS. We have not attempted to review the impact of lowered skin or body temperature on drug delivery from these systems. There may be circumstances when a patient might wear a TDS on a region of skin transiently exposed to relatively cold (even freezing) temperatures. Based upon the relationship between temperature and TDS drug delivery in the normal to high temperature range, transdermal drug delivery would likely be reduced at colder temperatures. Although low temperatures are not expected to lead to a drug overdose, they could potentially lead to under-dosing of topical or transdermal drugs. This is somewhat speculative and currently inconclusive because of the very limited literature describing the effects of cooling on transdermal and topical drug delivery. A critical review of the effects of lowered temperature on transdermal and topical drug delivery is beyond the scope of this work.
Go to:
2. Thermoregulation and heat effects on the temperature of the body and the skin
2.1. Thermoregulation
Thermoregulation plays an important role in maintaining the physiological homeostasis during physical exercise as well as at rest. Human body temperature is controlled by the thermoregulatory center in the hypothalamus, which responds to signals from the receptors in the hypothalamus and in the skin. The receptors in the hypothalamus monitor the internal (core) body temperature while the receptors in the skin monitor the external temperature. Through the use of feedback control, the human body can make thermal adjustments so that body temperature is maintained in a normal range. For example, stress from high temperatures can stimulate cutaneous vasodilation caused by autonomic smooth muscle relaxation in the blood vessels, sweating, and/or the modulation of adrenaline and thyroxine secretion from adrenal and thyroid glands, respectively. These physiological responses to heat can work in concert to distribute heat from the body core to the extremities and the skin surface. At the skin surface, heat can be dissipated through conduction, convection, radiation, and water evaporation,[5–7] and these thermoregulatory cooling mechanisms can be complemented by a reduction in metabolic heat production.
2.1.1. Cutaneous vasodilation and skin blood flow
2.1.1.1. Systemic exposure to heat and internal heat sources
Thermoregulatory vasodilation is vital to maintain normal body temperatures during heat exposure. Resting skin blood flow in a thermoneutral environment is approximately 0.25 L/min, which dissipates the 80–90 kcal/h of metabolic heat produced during rest. However, to modulate thermoregulation under conditions of elevated temperature, the skin blood flow can increase to 6–8 L/min during severe hyperthermia.[8] Cutaneous vasodilation, controlled by both nerve reflexes and local factors,[9] is effective at facilitating heat loss and thereby cooling the body. The reflex control of skin blood flow is mediated by two types of sympathetic nerves (i.e. sympathetic adrenergic vasoconstrictor nerves and sympathetic vasodilator nerves). The sympathetic vasodilator system is activated when the internal temperature or skin temperature increases beyond its threshold for cutaneous vasodilation. Factors that influence the threshold (and the sensitivity) of cutaneous vasodilation include heat acclimation, exercise training, circadian rhythm, and the production of nitric oxide from whole body heat stress.[8]
2.1.1.2. Local exposure to heat and external heat sources
Locally applied heat can increase the skin blood flow at the site of heat application. Short heat application (43°C for 60 s) was reported to cause significant cutaneous hyperemia with up to a twofold increase in skin perfusion and a 5°C increase in skin temperature, lasting up to 15 min from a single heat application.[10] As much as a ninefold increase in local blood flow was also reported in response to a rise of 9–13°C in skin temperature.[11,12] During local heating of the skin, factors such as local skin temperature contribute directly to the control of local skin blood flow, complementing the reflex neural control of skin blood flow that occurs via the sympathetic vasodilator nerves and any other contributing factors such as nitric oxide production.[13] The local sensory nerves are temperature sensitive and it has been reported that the activation of local nerves at temperatures ranging from 29°C to 40°C contributed to local vasodilation.[8,14] Charkoudian [8] characterized a typical cutaneous vasodilation pattern during 30 min of local skin heating at a skin temperature of 42°C, in which the skin blood flow rapidly increased in the first 3–5 min, decreased moderately, and then slowly increased to a maximum after 25–30 min of heating.[8,9,15,16] The activation of local sensory nerves and nitric oxide were the predominant contributors to the initial (rapid) and the subsequent (slow) increases in the skin blood flow, respectively.
The extent of increased skin blood flow is influenced by the skin temperature during local heating. A study of the relationship between forearm blood flow and local skin temperature showed that the increases in the skin blood flow were small between 20°C and 35°C, significant at 37°C and above, and maximal at approximately 42°C.[17] Similar observations were reported in other studies.[18,19] A later study confirmed that maximal vasodilation in the skin was reached when the skin temperature was maintained at 42°C.[9]
2.1.2. Sweating and water evaporation
The endothermic evaporation of sweat decreases the skin temperature, resulting in the cooling of the blood in the dilated skin vessels and the body. Sweating is regulated by internal body temperature as well as skin temperature. Sweat secretion and evaporation are also influenced by the environmental temperature and humidity. In a dry environment, the sweat evaporates almost immediately following secretion. This process is suppressed in a hot humid environment, with the consequence that the evaporative heat loss is less efficient and does not effectively cool the skin. One study [20] determined the skin temperature during a 45 min rest followed by 45 min exercises in a hot environment with normal humidity (49.5°C and 32% relative humidity (RH)). This study showed that the skin temperature increased rapidly during the first 20 min and then gradually to 37°C during the last 25 min of rest. During exercise, the skin temperature increased linearly from 5 min after the start of exercises and reached 39.1–39.8°C at the end of the exercises. An additional study was conducted on one subject during 45 min exercises in dry (15% RH) and normal (32% RH) environment at 49.5°C and reported that the skin temperatures were 37.5°C and 38.4°C in dry and normal environments, respectively.[20]
2.2. Skin temperature during heat exposure
Table 1 summarizes the skin temperatures during heat exposure under different conditions studied previously. Despite heat exposure and physical exercise, in most of the studies, the skin temperature does not exceed 43°C. For example, the mean skin temperature increased to 40–41°C during sauna bathing in a hot environment with an air temperature of 80–100°C.[21] A controlled heat-aided drug delivery (CHADD) system was reported to increase the skin temperature to approximately 41°C. [22,23] Independently, skin temperatures were reported to vary between 33°C and 40°C during exercises in a hot environment, depending on the RH of the environment. [20,24,25] Collectively, these findings suggest that a maximal skin temperature of approximately 42–43°C is most relevant for studying heat effects with topical and transdermal dosage forms.
Table 1
Skin temperatures during in vivo heat exposure studies.
Reference Study objective Heat application Skin temperature
[24] Uptake of glyceryl trinitrate Exercise 20 min; sauna air temperature 90°C 20 min Exercise: 33.3°C; sauna: 37.6– 38.1°C
[22] Transdermal delivery of fentanyl CHADD 4 h 41 ± 1°C
[26] Serum fentanyl concentrations during treatment of transdermal patches Electric heating pad 0–10 h and 26–36 h post-dosing 36–37°C
[23] Transdermal delivery of testosterone CHADD 4 h 41 ± 1°C
[12] Transdermal delivery of nicotine Local controlled heat 43°C 1 min every 5 min intervals for 30 min 43 ± 0.2°C
[27] Pharmacokinetic studies of granisetron transdermal system A heating pad over the transdermal system Around 42°C
[20] Thermoregulation Rest or exercise in a hot chamber of 49.5°C, 15% or 32% relative humidity 37°C at rest and 39.1–39.8°C during exercise
[25] Thermoregulation Three 20 min exercises followed by 7 min rest periods in hot and dry conditions (41 ± 1°C and 21% relative humidity) 31–32°C before exercise and
37–38°C at the end of exercise
[21] Thermoregulation Sauna air temperature 80–100°C, 5–20 min sessions 40–41°C
[9] Cutaneous vasodilation A water-perfused suit to control local temperatures from 18°C to 42°C 18–42°C
[16] Cutaneous vasodilation Peritemp local heating unit temperature at 42°C 50–80 min or increased from 33°C to 42°C at a rate of 0.5°C every 5 s 39–40°C
[13] Cutaneous vasodilation Local heating to 41°C by a special laser-Doppler flowmetry holder 41°C
[15] Cutaneous vasodilation Local heating to 42.5°C 30 min by a special laser-Doppler flowmetry holder 42.5°C
[14] Local thermal control of skin blood flow A Peltier cooling/heating device to change skin temperature between 20°C and 42°C 20–42°C
[28] Plaster splint application Plaster splint application in conjunction with the use of pillows or blankets 41–45°C
Open in a separate window
CHADD: controlled heat-aided drug delivery.
2.3. Body and skin temperature tolerance
The deviation of human body core temperatures by 3.5°C higher than the normal body temperature of 37°C can result in physiological impairments and even death.[7] High skin temperature can cause pain and may result in vasoconstriction.[8,12] The first phase transition of the skin SC lipids begins to occur around 40°C [29] and skin barrier function is compromised at high temperatures.[11] Brief heating to high temperature (i.e. <1 s exposure and >100°C) has been found to increase skin permeability by causing thermal damage to the SC without damaging deeper tissues.[30] Thermal exposure over 40°C for an extended period of time may cause thermal injury to skin and can cause burns.[28,31] Thermal conditions that cause skin burns are a function of the time and potentially the method of heat exposure as well as the skin temperature, and a skin temperature above 42°C should typically be avoided when studying heat effects.[32] Prolonged exposure of skin to 43°C or higher could lead to blister formation.[33] A physiologically tolerable temperature of 40°C has been proposed previously,[34] and as discussed in the preceding section, it may not be clinically relevant to study heat effects at skin temperatures higher than 42–43°C.
Go to:
3. Heat effects on dermal clearance
Local skin perfusion can be significantly increased during heat application and, in turn, can affect dermal clearance of drugs delivered by topical or transdermal administration. Reducing the rate of blood flow in the skin (i.e. reducing dermal clearance) was found to affect topical delivery of drugs by altering the residence time of drugs in the skin and underlying tissues.[35,36] Coadministration of vasoconstrictors has been shown to alter the absorption and distribution of topically applied drugs.[37] Therefore, blood flow changes in skin due to elevated skin temperatures can have an effect on relative processes of local and systemic drug distribution and absorption. It was suggested that the observed increase in plasma nitroglycerin concentrations in healthy subjects wearing nitroglycerin TDS during a 20 min sauna (air temperature 90°C and peak skin temperature 39°C) were partly due to cutaneous vasodilation.[24] In another study, the relationship between the skin blood flow and transdermal absorption of nitroglycerin was explored. The transdermal nitroglycerin systems were applied to the subjects’ upper arm and exposed to 15 min of local heat by an infrared heating bulb. The plasma drug concentrations increased when the skin blood flow increased due to heat exposure.[38] A recent clinical study on nicotine TDS proposed that the increased drug absorption after application of controlled heat (43°C) was largely due to enhanced microcirculation and local blood flow; the heat application was found to increase blood flow by approximately tenfold as compared with the blood flow at 32°C.[12] The results from these clinical studies suggest that local blood flow and dermal clearance of a drug are important considerations impacting transdermal and topical modes of dose administration, particularly under conditions of elevated temperature.
Go to:
4. Heat effects on TDS drug release and delivery through skin
4.1. Concerns related to heat effects on drug release from TDS
Application of heat can change the rate of drug release from a TDS. These systems are widely varied in design and their individual susceptibility to heat effects can also vary. Typical components of a matrix TDS include a backing film/membrane, drug dissolved and/or suspended in an adhesive matrix, and a release liner to protect the TDS until the drug product is dosed. The TDS formulation modulates the rate of drug release, drug partitioning into the SC, and drug diffusion/delivery into and through the skin. The goal of modern TDS product development is to optimize the rate of drug delivery per unit area (e.g. μg/h/cm2) and to minimize drug load. To achieve this goal, TDS formulation development typically involves the evaluation of a variety of different adhesives and excipients. The adhesives traditionally used in TDS are acrylates, silicones, and polyisobutylenes.[39] Some of the most commonly used excipients include mineral oil, colloidal silicon dioxide, dipropylene glycol, alcohol, and fatty acid esters. Under conditions of elevated temperature, the behaviors of these chemically distinct components, either individually or in a complex formulation mixture, are difficult to anticipate. Therefore, without experimental evaluation, it has been difficult to predict how drug release characteristics would change for a TDS under conditions of elevated temperature. As a further complexity, reservoir-type TDS contain an additional rate-limiting membrane which can also modulate the rate of release under conditions of elevated temperature exposure.
During the process of product development and approval, drug delivery from TDS is usually evaluated under conditions of relevant use, i.e. anticipated patient use without the application of heat or additional stress on the system. Drug manufacturers may also evaluate drug release from TDS under conditions of elevated temperature and incorporate corresponding cautionary statements in TDS product labels whenever it is anticipated or observed that exposure to elevated temperature could lead to higher drug plasma levels. Examples of TDS products that include warnings in product labels are those containing buprenorphine, fentanyl, granisetron, and methylphenidate, among others. This issue has special relevance for generic versions of TDS, which can contain different adhesives and/or excipients compared with those used in the reference listed drug (RLD), and a generic TDS may utilize an entirely different design than the RLD. Considering the growing body of evidence about heat effects on TDS performance, it is reasonable to expect that heat effect evaluations will continue to be needed. As such, the development of clinically relevant in vitro methods, perhaps combined with computational modeling of activation energies described later in this review, could greatly facilitate the routine evaluation of the comparative drug release and delivery profiles from generic TDS and their RLD products under conditions of elevated temperature exposure.
4.2. Effects of heat on skin permeation under steady-state conditions
Drug plasma concentrations are proportional to the rate of drug permeation across the skin at steady state in vivo, when the drug follows linear pharmacokinetics with zero-order delivery from a TDS. Hence, skin permeation rate or skin permeability can provide useful information as an initial estimate of the effect of skin permeability enhancement on plasma concentration in the context of transdermal delivery. The effects of heat on skin permeability were investigated as early as the 1960s. Scheuplein investigated the effects of temperature on the permeation of water through skin and noted the different permeation behaviors of water at different temperatures.[40] Blank et al. examined the effects of temperature on the transport of nonelectrolytes across the skin and found that polar and nonpolar molecules appeared to diffuse through the epidermis by different molecular mechanisms characterized by different activation energies.[41] Cornwell and Barry studied temperature dependence of skin conductivity and permeation and found significant temperature effects influencing these two properties.[42] In that study, two distinctive skin transport mechanisms were observed: (a) the activation energy of ion permeation across the skin was consistent with a mechanism whereby the ions primarily diffuse across an aqueous polar pathway in the skin and (b) the activation energy of 5-fluorouracil diffusion across the skin was consistent with a mechanism of solute transport across a lipid barrier. Later, Peck et al. compared the temperature dependence of skin permeation of urea, as a model polar permeant, with that of corticosterone, as a model lipophilic permeant, and showed a higher activation energy of skin transport for corticosterone than for urea.[43]
It is generally accepted that the increased skin permeation observed in situations of elevated temperature is primarily related to the increased diffusivity, partitioning, and solubility of drugs in the SC at the elevated temperatures. Both increased partitioning of lidocaine base into the epidermis and increased epidermal diffusion at 45°C as compared with that at 32°C were observed in a study attempting to elucidate how drug release, partitioning, and epidermal diffusion responded to changes in local temperature.[11] Additionally, heat may “dilate’ the skin penetration pathways and increase drug solubility in the skin, leading to enhanced skin absorption.[44] Recently, Mitragotri summarized the activation energies of more than 30 molecules in the literature and analyzed their relationships with the molecular properties.[45] The activation energies describe the nature of the transport barrier of a membrane and correspond to the changes in membrane diffusivity and membrane partitioning of the permeants under the influence of temperature. The activation energies for various permeants in accordance with the Arrhenius equation are listed in Table 2, and the changes in permeability coefficients as ratios from 32°C to 37°C and 42°C were calculated using the activation energies of the permeants presented by Mitragotri. [45] Only human skin data are included in Table 2. The activation energy values range from 4 to 23 kcal/mol, and the permeability coefficients for these compounds of different molecular sizes and lipophilicities increase by as much as 1.9-fold with a 5°C increase above normal skin temperature of 32°C, and by as much as 3.4-fold with a 10°C increase from 32°C to 42°C. Similar results were reported for other compounds; e.g., with activation energies of 13–20 kcal/mol for methyl paraben, butyl paraben, and caffeine, approximately twofold increases in the epidermal fluxes of these compounds from their saturated suspensions were observed with an increase of 7–8°C in the temperature range of 23–45°C.[29]
Table 2
Calculated values of permeability enhancement due to changes in temperature based on activation energies of permeants.
Permeant Activation energy (kcal/mol)a Ratio of permeability at 37°C to 32°C Ratio of permeability at 42°C to 32°C
Acetylsalicylic acid 20.3 1.7 2.9
Butanol (n-butanol) 16.7 1.6 2.4
Butanone (2-butanone) 16.1 1.5 2.3
Butyl paraben 20.3 1.7 2.9
p-Bromophenol 8.8 1.3 1.6
Caffeine 12.7 1.4 1.9
Carbon disulfide 16.9 1.6 2.4
Chlorocresol 10.3 1.3 1.7
o-Chlorophenol 9.6 1.3 1.7
Corticosterone 23.2 1.9 3.4
m-Cresol 13.6 1.4 2.0
o-Cresol 12.8 1.4 2.0
p-Cresol 13.7 1.4 2.1
1,1-Dichloropropanone 11.2 1.3 1.8
Ethyl ether 16.1 1.5 2.3
Ethanol 19.6 1.7 2.8
Ethoxy ethanol 20.1 1.7 2.9
5-Fluorouracil 23.4 1.9 3.4
Glycopyrrolate 17.7 1.6 2.5
Heptanol 9.9 1.3 1.7
Hexanol 10.9 1.3 1.8
Ion conductivity 4.1 1.1 1.2
Mannitol 8.8 1.3 1.6
Methyl paraben 15.5 1.5 2.3
Methylsalicylic acid 13.7 1.4 2.1
Naphthol 9.8 1.3 1.7
m-Nitrophenol 13.3 1.4 2.0
Octanol 10.0 1.3 1.7
Pentanol 16.5 1.6 2.4
Phenol 14.4 1.5 2.1
Propanol 16.5 1.6 2.4
Resorcinol 17.8 1.6 2.5
Sarin 16.9 1.6 2.4
Tetraethylammonium 8.3 1.2 1.5
Thiourea 16.2 1.5 2.3
Thymol 12.6 1.4 1.9
2,4,6-Trichlorophenol 9.1 1.3 1.6
Urea 7.1 1.2 1.4
Water 14.6 1.5 2.1
Open in a separate window
aData from [45] in accordance with the Arrhenius equation.
4.3. Effects of heat on transdermal and topical drug delivery systems
4.3.1. Effects of heat on transdermal drug delivery in vivo
Myriad studies of the effects of heat application on in vivo drug absorption from TDS and their findings are summarized in Table 3. In these studies, the plasma or serum peak drug concentrations and areas under the curve (AUCs) were often increased under conditions of elevated temperature. However, significant heat effects were not always observed. For example, in one study with an ethinyl estradiol and norelgestromin TDS, no significant heat effect was observed.[46] Likewise, the evaluation of a granisetron TDS using a heating pad indicated that although there was a small enhancement in flux, no significant changes were noted in the pharmacokinetics of the drug in humans.[27]
Table 3
Summary of in vivo studies for transdermal and topical delivery systems under conditions of elevated temperature.
Reference Drug name Heat application Results
Transdermal delivery systems
[47] Clonidine Bath 40°C 5 min daily; hot weather (summer versus winter) Hot bath had no effects on peak plasma concentrations or AUC; however, peak plasma concentrations and AUC tended to be higher in the summer trial
[48] Ethinyl estradiol/ levonorgestrel Dry sauna 76–82°C 10 min/day for 7 days; whirlpool 39–41°C 10 min/day for 7 days; treadmill 20–30 min/day for 7 days Decreased the mean peak concentration and AUC; slightly lower mean drug concentrations
[46] Ethinyl estradiol/norelgestromin Sauna 76–82°C 10 min daily for 7 days; whirlpool 39–41°C 10 min daily for 7 days; treadmill 20–30 min daily for 7 days Plasma concentrations remained within the reference range; no heat effect was observed
[27] Granisetron A heating pad was applied over the patch during either first or second patch application; 4.5 h daily for 5 days No overall effects of heat on pharmacokinetics of transdermal granisetron; while small increases in granisetron concentration during heat application were observed, the concentration quickly returned to without heat levels once the heat was removed
[22] Fentanyl CHADD 4 h Increased mean peak concentration and AUC for the 4 h period of heat application
[26] Fentanyl Electric heating pad to produce skin temperature 36–37°C, 0–10 h and 26–36 h post-dosing A similar effect on both matrix and reservoir systems: increased serum concentrations and AUC for the first 10 h
[49] Fentanyl Controlled heat to produce temperature 42 ± 2°C for 60 min; 0–4 h application During the first 4 h, three times higher peak concentration and AUC for the heated group than for the control without heat
[24] Glyceryl trinitrate Exercise 20 min; sauna 20 min at sauna air temperature 90°C Increased mean plasma concentrations
[50] Glyceryl trinitrate Exercise 20 min three times after patch application, renewal, and removal Increased peak plasma concentrations
[38] Nitroglycerin Local heating 15 min with an infrared bulb About twofold increase in mean plasma concentration
[12] Nicotine Local controlled heat 43°C 1 min every 5 min intervals for 30 min Up to 13-fold increase in nicotine uptake
[51] Nicotine Sauna bath 82°C, 28% RH, three 10 min periods separated by two 5 min breaks Increased peak plasma concentrations, AUC between 0 and 1 h, nicotine absorbed, and mean plasma concentrations; no significant difference in AUC between 0 and 3 h
[52] Nicotine Exercise 1 h at 8 h after patch application Exercise increased tissue concentration but had no effect on plasma concentration. A similar effect was observed for two patch products
[53] Nicotine Exercise 20 min at 11 h after patch application Increased plasma concentration during exercise
[23] Testosterone CHADD 4 h Significant increases in peak concentration, AUC with heat application
Topical delivery systems
[54] Lidocaine/tetracaine Four heated patches for 2, 4, and 12 h Increased plasma concentrations during the first 2 hours of application; time-normalized AUC showed no difference or lower between 2 and 12 h of application
Open in a separate window
AUC: areas under the curve; CHADD: controlled heat-aided drug delivery.
The fentanyl TDS is one of the most widely investigated transdermal products, and a relatively large body of in vivo data characterizing heat effects with fentanyl TDS is available in the literature. The scientific interest in characterizing heat effects with fentanyl TDS is, in part, because heat may be used in combination with the fentanyl TDS for the treatment of pain, and particularly because fentanyl has a narrow therapeutic index and elevated fentanyl delivery could be toxic or fatal. The CHADD system contains a heat-generating element and produces heat when exposed to air. It can be applied on a transdermal or topical system to enhance drug delivery. The impact of local heat on the systemic delivery of fentanyl from TDS was previously assessed using a CHADD patch as a heat source.[22] The CHADD patch is designed to produce heat for 4 h and the heat passing through the fentanyl TDS increases skin temperature to 41 ± 1°C. The results show that the mean peak plasma concentration and mean AUC in healthy subjects were significantly increased during the heat application period. Additionally, using the CHADD patch could produce rapid increases in serum fentanyl concentrations and shorten the time needed to reach the therapeutic concentration.[49] Moore et al. recently evaluated the effects of a heating pad on serum fentanyl concentrations with reservoir and matrix transdermal fentanyl systems.[26] The results from this study indicate that the external heating pad had similar effects on both matrix and reservoir systems.
Similar heat effects on transdermal drug absorption were also observed for drugs formulated in dosage forms other than TDS. The effects of heat exposure and exercise on transdermal absorption of methyl salicylate were investigated in healthy subjects performing 45 min exercises every hour over 6 h at 22°C and 40°C, after the drug was smeared over the skin.[55] It was found that plasma drug concentrations were significantly higher during heat exposure and exercise.
4.3.2. Effects of heat on transdermal and topical drug delivery in vitro
Various exploratory in vitro studies of heat effects on drug release and skin permeation from TDS and topical delivery systems are summarized in Table 4. For example, internally heated TDS of diclofenac sodium and lidocaine hydrochloride were tested in vitro with synthetic membranes using a dissolution apparatus or Franz diffusion cells.[34] These TDS contained a heating element that generated heat to rapidly increase the TDS temperatures to approximately 40°C. The results from this study show that drug release from these drug products was significantly increased with heat application. Similarly, external heating was found to increase the transdermal flux of isosorbide dinitrate from a TDS by 2.5 times as compared to that without heating, but in another example, heating had minimal effect on transdermal flux of oxybutynin under similar conditions.[56] In yet another exploratory study,[11] the skin permeation of lidocaine from a suspension was increased when the skin temperature was increased from 32°C to 45°C, but no heat effect on the flux was observed between 27°C and 32°C. These results illustrate that the effects of heat on transdermal and topical drug delivery may not be consistently observed in vitro, potentially due to the design of the in vitro study and/ or the design of the drug delivery systems. Hence, it remains uncertain whether these observed effects can be translated into clinically meaningful changes in drug delivery.
Table 4
Summary of in vitro study conditions for transdermal and topical delivery systems under elevated temperature.
Reference Formulation information Heat application Transport devices/parameters/skins Results
Transdermal delivery systems
[56] Transdermal delivery systems containing 24 mg oxybutynin per patch in size of 26 cm2 or 40 mg isosorbide dinitrate per patch in size of 6.35 × 6.35 cm2 Group 1: no temperature control to the donor chamber, i.e. room temperature
Groups 2 and 3: thermostatic water was circulated on the surface of the transdermal delivery system to maintain the patch surface temperatures at 36°C and 45°C, respectively
Receptor temperature was maintained at 37°C by circulating thermostatic water
Experimental duration: 60 h Franz diffusion cells with an effective diffusion area of 1.767 cm2
Human cadaver skins (stored at –60°C) were thawed at room temperature and the epidermal membranes of 500 μm in thickness obtained by a dermatome; 7 or 8 pieces of epidermal membrane from four donors were tested at each temperature
A three-layered stack consisting of the patch, epidermal membrane, and support membrane (Nuclepore Track-Etch Membrane, Whatman) was mounted on the diffusion cells
Receptor was pH 6.8 (for oxybutynin) or pH 7.4 (for isosorbide dinitrate) phosphate buffered saline containing 0.02% sodium azide and infused at 3 mL/h; the receptor samples were taken at 1.5 h intervals over 60 h The fluxes of oxybutynin at 36°C and 45°C were approximately 1.2-fold higher than that at room temperature; the fluxes of isosorbide dinitrate with heating were 2.6–2.8 times higher than that without heating
[57] Fentanyl reservoir and matrix patches at 2.5 μg/h strength containing 2.5 mg per patch in sizes of 10 cm2 for the reservoir patch and 6.25 cm2 for the matrix patch The temperature of the dissolution medium was set at 32°C or 40°C for up to 72 h US Pharmacopoeia dissolution apparatus 5
Full-thickness human cadaver skins excised within 24 h postmortem were stored at –20°C and used within 3 months of storage; the skin samples were thawed for 2 h at room temperature and subjected to heat separation to obtain epidermis membranes for skin integrity tests by measuring transepidermal water loss and uses in transport studies
The dissolution medium consisted of 600 mL of Hank’s balanced salts solution
Paddle rotation speed was 50 rpm
Three to six replicates were performed for each experiment Drug release and skin permeation at normal skin temperature was comparable for both patches; the permeation rate at 40°C was twice that at 32°C over the first 24 h in both systems; the total drug permeation in 72 h was higher in the reservoir patch
[34] Heated transdermal patches of ketoprofen, diclofenac sodium, or lidocaine hydrochloride Dissolution apparatus: the temperature of the dissolution medium was set at 32–42°C for 1 h
Franz diffusion cells: receptor 32°C and donor temperature was increased up to 40°C, which was determined by a heat element contained in the patch Dissolution apparatus with an enhancer cell; 200 mL deionized water as the dissolution medium; the gel-loaded enhancer cells were rotated at 50 rpm
Franz diffusion cells; 0.45 μm cellulose acetate membrane as a support; 12 mL deionized water as the receptor solution and the patch containing 1 g gel as the donor; samples of 1 mL were withdrawn from the receptor at 5 min intervals Flux increased 2.5–3-fold using the heated patches compared with the nonheated gels
Topical delivery systems
[11] Lidocaine suspension The skin temperature was maintained at 27°C, 32°C, 37°C, and 45°C for 2 h using a water bath Franz diffusion cells with an effective diffusion area of 2 cm2 and receiver volume of 10 mL Human epidermal sheet was obtained by heat separation
The receiver solution was pH 7.3 phosphate-buffered saline (0.15 M); receiver samples of 1 mL were taken at 0, 10, 20, 30, 40, 50, 60, 90, and 120 min No significant difference in the steady-state flux between 27°C and 32°C; significant increases in the steady-state flux from 32°C to 45°C
[29] Saturated suspensions of methyl paraben, butyl paraben, and caffeine The receptor temperature was maintained at 23°C, 30°C, 37°C, and 45°C for up to 6 h using a water bath Franz diffusion cells with a diffusion area of 0.6 cm2 and receptor volume of 1.8 mL
Fresh, surgically excised human skin was obtained from a female donor and the abdominal sections of the skin from this donor were used throughout the study; epidermal sheets were obtained by heat separation after removal of subcutaneous fat; the epidermal sheet filter paper (Whatman no. 1) assembly was used
The donor was 200 μL suspensions and the receptor was pH 7.4 phosphate buffered saline; receptor samples were taken at 30, 60, 90, 120, 180, and 240 min About twofold increase in flux was observed for every 7–8°C increase in receptor temperature
Open in a separate window
Different TDS design features could result in different heat effects on transdermal drug delivery. Prodduturi et al. investigated the effects of heat on fentanyl release and permeation through heat-separated human epidermis from a reservoir-type TDS and a matrix-type TDS. [57] It was found that fentanyl release from both TDS was significantly increased at 40°C compared with the release observed at normal skin temperature of 32°C. The drug release rate was much higher from the matrix TDS than from the reservoir TDS under both temperature conditions. At 32°C, about 80% of fentanyl was released in 72 h from the reservoir-based TDS and the same percent of fentanyl was released in 5 h from the matrix TDS. At 40°C, the time required for 80% drug release was shortened to 18 h for the reservoir TDS and 2 h for the matrix TDS, respectively. The observed difference in kinetics of drug release was attributed to the difference in TDS designs. For example, a continuous depletion of the alcohol contained in the reservoir TDS could account for the complex kinetics of drug release from these TDS. This suggests that heat effects on drug release from transdermal systems could vary with the TDS designs (reservoir or matrix type) as well as with the excipients (solvents and/or enhancers) used in the TDS. It is also noteworthy that the reservoir TDS have larger sizes (10–40 cm2) than the matrix TDS (6.25–25 cm2) at each dosing strength; this affects the amount of drug released per unit TDS area. Although drug permeation through heat separated human epidermis in vitro was found to be equivalent at normal skin temperature of 32°C for the reservoir and matrix fentanyl TDS, the drug permeation profiles of these TDS were different at 40°C. Specifically, the fentanyl skin permeation rate for these two types of TDS at 40°C increased by twofold in the first 24 h and then decreased over the next 48 h relative to their respective controls at 32°C. The overall amount of drug permeated in 72 h at 40°C was higher for the reservoir TDS than the matrix TDS.
4.3.3. Effects of heat on topical drug delivery in vivo
Local controlled heat has been used to enhance topical drug delivery. Heated patches of lidocaine/tetracaine are indicated for use on intact skin to provide local dermal analgesia for superficial venous access and superficial dermatological procedures. The lidocaine/ tetracaine heated patches contain an oxygen-activated heating component designed to enhance topical drug delivery. The heated patches are typically applied to the skin for 20–30 min prior to surgical procedures. The heating element generates a controlled level of heating that ranges from approximately 36°C to 40°C for about 2 h.[58] Marriott et al. studied these heated patches in healthy volunteers during 2, 4, and 12 h applications. [54] The plasma drug concentrations were observed to increase during the first 2 h for all heated patch groups. Compared with the nonheated patch application, the mean plasma drug concentrations were approximately fivefold and threefold higher, respectively, following 30 and 60 min applications of the heated patches. However, the time-normalized AUC was similar or lower for the 4 and 12 h heated patch applications as compared with the 2 h application group, suggesting that the in vivo drug delivery rate was diminished after 4 h application of the heated patches, perhaps due to accelerated depletion of the drug load and the driving force for the delivery.
4.4. Experimental conditions for heat effect studies in vitro and in vivo
4.4.1. In vitro studies
As shown in Table 4, while there have been similarities in the in vitro conditions for studying transdermal and topical drug delivery systems under the influence of temperature, there has been no standard testing condition used in the heat application studies reported to date. The testing conditions vary with respect to temperatures tested, heating source, schedules of elevated temperature application or duration, and in vitro apparatus design. For example, the effects of temperature on in vitro drug release and skin permeation from suspensions and TDS have been investigated across a temperature range of 23–45°C, and using dissolution apparatus, side-by-side diffusion cells, or vertical Franz diffusion cells in the studies summarized in this review.
4.4.2. In vivo studies
As seen with the in vitro study conditions, there has been no standard testing protocol used in heat effect studies of transdermal and topical delivery systems in vivo. The heat sources used in the in vivo heat application studies include electric pads, electric blankets, sauna, whirlpool, heated water bath, infrared bulb, and exercise.[24,26,38,46,51] As shown in Table 3, the testing conditions also vary among the different clinical studies conducted by different research groups. For example, the durations of heat applications ranged from 5 min to 10 h; the temperatures of heating sources were 76–90°C for the sauna, 39–41°C for the whirlpool, 40°C for the heated water bath, and 42–43°C for local controlled heat. As the skin temperature was not monitored precisely in several of the reported heat effect studies in vivo, it is difficult to design in vitro study conditions that could match the in vivo study designs in order to be correlated with the in vivo data currently available.
Ultimately, while there have been several in vitro and in vivo studies of drug delivery from transdermal and topical drug products under the influence of elevated temperature, discrepancies in study design and lacunae in methodological reporting among the different studies undermine the evaluation of in vitro–in vivo correlations (IVIVC). Instead, further research with matched in vitro and in vivo studies using harmonized protocols for heat exposure are needed to better characterize heat effects with different TDS and to evaluate whether an in vitro model can be correlated with and be predictive of the TDS heat effects observed in humans in vivo.
Go to:
5. Conclusion
Human thermoregulation and heat effects on skin blood flow, drug release, drug permeation, and the corresponding pharmacokinetics of drug delivery from transdermal and topical systems have been reviewed. Elevated temperature significantly increases skin blood flow as well as dermal clearance. The effects of heat on drug release and skin permeation are complex, depending on the nature of heat application, the design of the drug delivery system, and the product’s characteristics. Nonetheless, the current body of literature suggests that heat exposure increases the in vivo dermal absorption of many drugs from transdermal or topical delivery systems.
Go to:
6. Expert opinion
Heat exposure can have a significant influence on transdermal and topical delivery of drugs. The mechanisms underlying these effects include increased drug release from the dosage form, increased drug permeation into and across the skin, increased skin perfusion, and increased dermal clearance to systemic circulation. The extent of the effects of heat exposure on in vivo drug absorption, pharmacodynamics, and possible adverse events associated with a dermatological product such as TDS is also expected to be affected by the physicochemical and pharmacological properties of the drug(s) and the drug delivery system formulation design. Therefore, evaluation of drug delivery under various thermal conditions remains an important part of development processes for topical and transdermal systems. The mechanisms underlying heat effects on transdermal and topical drug delivery could apply to other drug products applied to the skin.
Characterizing and predicting heat effects on transdermal and topical drug products are of interest to support the regulatory evaluation of these dosage forms. IVIVC of the heat effects characterized for transdermal and topical products have yet to be established. Although heat effects have been studied for some transdermal and topical drug products, due to the different testing conditions and protocols used in the in vitro and in vivo studies conducted by different research groups, it is difficult to compare the data among these groups with the intent to develop an IVIVC that can effectively predict the influence of heat on transdermal and topical drug delivery, even for TDS of the same drug molecule.
It appears that the skin temperature during heat exposure is well controlled by thermoregulation, and skin temperatures of 43°C and above can lead to burns and intolerable pain. Patients generally avoid long-term skin exposure to a temperature higher than 43°C, and the skin temperature encountered during transdermal or topical drug delivery is likely below this temperature; that is, a study of the effect of heat can be conducted within the 32°C to ~42°C range. However, the duration and frequency of heat exposure have not been standardized in heat effect studies of transdermal and topical drug products. Heat application protocols in these studies should reasonably mimic heat exposure situations that patients would normally encounter in the course of product wear. Also, the prescribed application duration of the particular product should be considered as part of the heat effect study design.
In this review of the literature, in vivo as well as in vitro data have been summarized. The study designs used in those studies are diverse, and it is difficult to correlate in vitro and in vivo data. Furthermore, key study parameters such as the local temperature of the skin are missing from the available data sets in several of the reported studies, making it difficult to correlate the data. For some studies, clinical data before and after heat exposure (i.e. characterizing the change in the amount of drug delivered) are available, but very few study data sets in these studies contain data from the period during heat application. Drug plasma concentration profile data during heat application are important for studying the mechanisms of heat on in vivo drug absorption, as it has been reported that skin temperature, local blood flow, and subsequent drug absorption can change drastically upon the removal of heat exposure. The availability of in vivo data sets that can be used to establish an IVIVC is very limited. It is, therefore, recommended that such studies be adequately designed to allow researchers to obtain drug concentration–time profiles in plasma during heat application.
It remains challenging to develop an in vitro study method to adequately characterize relevant heat effects on transdermal drug products. Although in vivo data for some TDS products are available in the literature, the in vitro testing conditions that appropriately model the in vivo conditions have not been identified. For example, the skin temperature and the duration and frequency of heat exposure that best describe the heat conditions encountered in practice have yet to be identified for the evaluation of heat effects in these in vitro studies. To mimic in vivo situations, the study design for the in vitro permeation test (IVPT) using excised human skin should match as closely as possible the conditions in the in vivo clinical use situation in order to establish an IVIVC (for which this model is otherwise known), specifically under conditions of elevated temperature. [59,60] This may include matching the heat source direction and temperature gradient, either from above the skin to mimic external sources of elevated temperature, or from beneath the skin using a heated receptor solution to mimic rises in body core temperature associated with strenuous exercise. In addition, the skin temperature in the IVPT study should be monitored and precisely controlled between the normal skin temperature of 32°C and the maximum elevated temperature of 42°C.
Other in vitro tests such as those with a dissolution apparatus or diffusion cells with synthetic membranes may have limitations detecting the changes in drug release, and would not be expected to predict the influence of drug permeation through the skin on drug bioavailability. Local skin blood flow and dermal clearance can play an important role in transdermal delivery in vivo during heat exposure.[12,24,38] Unfortunately, the existing in vitro study models are not well suited to study the effect of dermal clearance on transdermal absorption in vivo. As such, the development of a computational model to account for dermal clearance and for different elevated temperature exposure scenarios could theoretically complement IVPT results, and together may facilitate the prediction of transdermal drug delivery in vivo under the influence of different scenarios of elevated temperature. Such an approach could be a valuable tool to help characterize and distinguish different effects of elevated temperature on the performance of transdermal or topical products.
Article highlights
Human thermoregulation plays a key role in maintaining the physiological homeostasis during heat stress.
Elevated temperature significantly increases skin blood flow, which can play an important role in transdermal and dermal delivery.
Heat application affects both drug release from transdermal drug delivery systems and drug delivery into and across the skin.
There have been no standard testing conditions or protocols to evaluate the effect of heat on drug delivery across human skin.
The development of an in vitro model to adequately characterize relevant heat effects on the in vivo performance of transdermal or topical drug products involves several considerations, and further research is necessary to establish an in vitro–in vivo correlation.
This box summarizes key points contained in the article.
Go to:
Footnotes
Declaration of Interest
Funding for this work was made possible, in part, by the U.S. Food and Drug Administration through grant U01FD004942. The views expressed in this manuscript do not reflect the official policies of the U.S. Food and Drug Administration or the U.S. Department of Health and Human Services; nor does any mention of trade names, commercial practices, or organization imply endorsement by the United States Government. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Go to:
References
Papers of special note have been highlighted as:
* of interest
** of considerable interest
1. Newshan G. Heat-related toxicity with the fentanyl transdermal patch. J Pain Symptom Manage. 1998;16:277–278. [PubMed] [Google Scholar]
2. Frölich MA, Giannotti A, Modell JH, et al. Opioid overdose in a patient using a fentanyl patch during treatment with a warming blanket. Anesth Analg. 2001;93:647–648. [PubMed] [Google Scholar]
3. Sindali K, Sherry K, Sen S, et al. Life-threatening coma and full-thickness sunburn in a patient treated with transdermal fentanyl patches: a case report. J Med Case Rep. 2012;6:220. doi: 10.1186/1752-1947-6-220. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
4. Carter KA. Heat-associated increase in transdermal fentanyl absorption. Am J Health Syst Pharm. 2003;60:191–192. [PubMed] [Google Scholar]
5. Henriques FC, Moritz AR. Studies of thermal injury: I. The conduction of heat to and through skin and the temperatures attained therein. A theoretical and an experimental investigation. Am J Pathol. 1947;23:530–549. [PMC free article] [PubMed] [Google Scholar]
6. Xu F, Lu TJ, Seffen KA. Biothermomechanics of skin tissues. J Mech Phys Solids. 2008;56:1852–1884. doi: 10.1016/j.jmps.2007.11.011. [CrossRef] [Google Scholar]
7. Lim CL, Byrne C, Lee JK. Human thermoregulation and measurement of body temperature in exercise and clinical settings. Ann Acad Med Singapore. 2008;37:347–353. [PubMed] [Google Scholar]
8••. Charkoudian N. Skin blood flow in adult human thermoregulation: how it works, when it does not, and why. Mayo Clin Proc. 2003;78:603–12. doi: 10.4065/78.5.603. This is a comprehensive review article on skin blood flow in human thermoregulation. [PubMed] [CrossRef] [Google Scholar]
9. Pérgola PE, Kellogg DL, Jr, Johnson JM, et al. Role of sympathetic nerves in the vascular effects of local temperature in human forearm skin. Am J Physiol. 1993;265:H785–92. [PubMed] [Google Scholar]
10. Gazerani P, Arendt-Nielsen L. Cutaneous vasomotor reactions in response to controlled heat applied on various body regions of healthy humans: evaluation of time course and application parameters. Int J Physiol Pathophysiol Pharmacol. 2011;3:202–209. [PMC free article] [PubMed] [Google Scholar]
11•. Wood DG, Brown MB, Jones SA. Understanding heat facilitated drug transport across human epidermis. Eur J Pharm Biopharm. 2012;81:642–9. doi: 10.1016/j.ejpb.2012.03.019. This paper studied the effects of heat on drug release and permeation with a topical formulation. [PubMed] [CrossRef] [Google Scholar]
12. Petersen KK, Rousing ML, Jensen C, et al. Effect of local controlled heat on transdermal delivery of nicotine. Int J Physiol Pathophysiol Pharmacol. 2011;3:236–242. [PMC free article] [PubMed] [Google Scholar]
13. Kellogg DL, Jr, Liu Y, Kosiba IF, et al. Role of nitric oxide in the vascular effects of local warming of the skin in humans. J Appl Physiol. 1999;86:1185–1190. [PubMed] [Google Scholar]
14. Stephens DP, Charkoudian N, Benevento JM, et al. The influence of topical capsaicin on the local thermal control of skin blood flow in humans. Am J Physiol Regul Integr Comp Physiol. 2001;281:R894–901. [PubMed] [Google Scholar]
15. Charkoudian N, Eisenach JH, Atkinson JL, et al. Effects of chronic sympathectomy on locally mediated cutaneous vasodilation in humans. J Appl Physiol. 2002;92:685–690. [PubMed] [Google Scholar]
16. Minson CT, Berry LT, Joyner MJ. Nitric oxide and neurally mediated regulation of skin blood flow during local heating. J Appl Physiol. 2001;91:1619–1626. [PubMed] [Google Scholar]
17. Barcroft H, Edholm OG. The effect of temperature on blood flow and deep temperature in the human forearm. J Physiol. 1943;102:5–20. [PMC free article] [PubMed] [Google Scholar]
18. Taylor WF, Johnson JM, O’Leary D, et al. Effect of high local temperature on reflex cutaneous vasodilation. J Appl Physiol Respir Environ Exerc Physiol. 1984;57:191–196. [PubMed] [Google Scholar]
19. Johnson JM, O’Leary DS, Taylor WF, et al. Effect of local warming on forearm reactive hyperaemia. Clin Physiol. 1986;6:337–346. [PubMed] [Google Scholar]
20. Kabayashi K, Horvath SM, Diaz FJ, et al. Thermoregulation during rest and exercise in different postures in a hot humid environment. J Appl Physiol Respir Environ Exerc Physiol. 1980;48:999–1007. [PubMed] [Google Scholar]
21. Leppäluoto J. Human thermoregulation in sauna. Ann Clin Res. 1988;20:240–243. [PubMed] [Google Scholar]
22•. Shomaker TS, Zhang J, Ashburn MA. Assessing the impact of heat on the systemic delivery of fentanyl through the transdermal fentanyl delivery system. Pain Med. 2000;1:225–30. This paper examined the impact of heat on transdermal delivery of fentanyl in vivo. [PubMed] [Google Scholar]
23. Shomaker TS, Zhang J, Ashburn MA. A pilot study assessing the impact of heat on the transdermal delivery of testosterone. J Clin Pharmacol. 2001;41:677–682. [PubMed] [Google Scholar]
24. Barkve TF, Langseth-Manrique K, Bredesen JE, et al. Increased uptake of transdermal glyceryl trinitrate during physical exercise and during high ambient temperature. Am Heart J. 1986;112:537–541. [PubMed] [Google Scholar]
25. Inbar O, Morris N, Epstein Y, et al. Comparison of thermoregulatory responses to exercise in dry heat among prepubertal boys, young adults and older males. Exp Physiol. 2004;89:691–700. doi: 10.1113/expphysiol.2004.027979. [PubMed] [CrossRef] [Google Scholar]
26•. Moore KT, Sathyan G, Richarz U, et al. Randomized 5-treatment crossover study to assess the effects of external heat on serum fentanyl concentrations during treatment with transdermal fentanyl systems. J Clin Pharmacol. 2012;52:1174–85. doi: 10.1177/0091270011411710. This paper investigated the heat effect on serum fentanyl concentrations with transdermal delivery systems of different transdermal delivery systems (TDS) designs. [PubMed] [CrossRef] [Google Scholar]
27. Haislip S, Gilmore J, Howell J. Results from four pharmacokinetic studies of the granisetron transdermal system. Res Rep Transdermal Drug Deliv. 2013;2:19–26. [Google Scholar]
28. Shuler FD, Bates CM. Skin temperatures generated following plaster splint application. Orthopedics. 2013;36:364–367. doi: 10.3928/01477447-20130426-06. [PubMed] [CrossRef] [Google Scholar]
29. Akomeah F, Nazir T, Martin GP, et al. Effect of heat on the percutaneous absorption and skin retention of three model penetrants. Eur J Pharm Sci. 2004;21:337–345. [PubMed] [Google Scholar]
30. Park J-H, Lee J-W, Kim Y-C, et al. The effect of heat on skin permeability. Int J Pharm. 2008;359:94–103. doi: 10.1016/j.ijpharm.2008.03.032. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
31. Hutchinson MJ, Hutchinson MR. Factors contributing to the temperature beneath plaster or fiberglass cast material. J Orthop Surg Res. 2008;3:10. doi: 10.1186/1749-799X-3-10. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
32. Lawrence JC, Bull JP. Thermal conditions which cause skin burns. Eng Med. 1976;5:61–63. doi: 10.1243/EMED_JOUR_1976_005_023_02. [CrossRef] [Google Scholar]
33. Moritz AR, Henriques FC. Studies of thermal injury: II. The relative importance of time and surface temperature in the causation of cutaneous burns. Am J Pathol. 1947;23:695–720. [PMC free article] [PubMed] [Google Scholar]
34. Otto DP, de Villiers MM. The experimental evaluation and molecular dynamics simulation of a heat-enhanced transdermal delivery system. AAPS PharmSciTech. 2013;14:111–120. doi: 10.1208/s12249-012-9900-6. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
35. Cross SE, Thompson MJ, Roberts MS. Transdermal penetration of vasoconstrictors–present understanding and assessment of the human epidermal flux and retention of free bases and ion-pairs. Pharm Res. 2003;20:270–274. [PubMed] [Google Scholar]
36. Higaki K, Nakayama K, Suyama T, et al. Enhancement of topical delivery of drugs via direct penetration by reducing blood flow rate in skin. Int J Pharm. 2005;288:227–233. doi: 10.1016/j.ijpharm.2004.09.025. [PubMed] [CrossRef] [Google Scholar]
37•. Singh P, Roberts MS. Effects of vasoconstriction on dermal pharmacokinetics and local tissue distribution of compounds. J Pharm Sci. 1994;83:783–91. This paper studied the effect of skin blood flow on dermal absorption. [PubMed] [Google Scholar]
38. Klemsdal TO, Gjesdal K, Bredesen JE. Heating and cooling of the nitroglycerin patch application area modify the plasma level of nitroglycerin. Eur J Clin Pharmacol. 1992;43:625–628. [PubMed] [Google Scholar]
39. Tan HS, Pfister WR. Pressure-sensitive adhesives for transdermal drug delivery systems. Pharm Sci Technolo Today. 1999;2:60–69. [PubMed] [Google Scholar]
40••. Scheuplein RJ. Analysis of permeability data for the case of parallel diffusion pathways. Biophys J. 1966;6:1–17. doi: 10.1016/S0006-3495(66)86636-5. This is one of the first research articles studying heat effect on skin permeability. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
41. Blank IH, Scheuplein RJ, MacFarlane DJ. Mechanism of percutaneous absorption. 3. The effect of temperature on the transport of non-electrolytes across the skin. J Invest Dermatol. 1967;49:582–589. [PubMed] [Google Scholar]
42. Cornwell PA, Barry BW. The routes of penetration of ions and 5-fluorouracil across human skin and the mechanisms of action of terpene skin penetration enhancers. Int J Pharm. 1993;94:189–194. doi: 10.1016/0378-5173(93)90023-9. [CrossRef] [Google Scholar]
43. Peck KD, Ghanem AH, Higuchi WI. The effect of temperature upon the permeation of polar and ionic solutes through human epidermal membrane. J Pharm Sci. 1995;84:975–982. [PubMed] [Google Scholar]
44. Hull W. Heat-enhanced transdermal drug delivery: a survey paper. J Appl Res. 2002;2:69–76. [Google Scholar]
45••. Mitragotri S. Temperature dependence of skin permeability to hydrophilic and hydrophobic solutes. J Pharm Sci. 2007;96:1832–9. doi: 10.1002/jps.20793. This paper summarized literature data on activation energies. [PubMed] [CrossRef] [Google Scholar]
46. Abrams LS, Skee DM, Natarajan J, et al. Pharmacokinetics of norelgestromin and ethinyl estradiol delivered by a contraceptive patch (Ortho Evra/Evra) under conditions of heat, humidity, and exercise. J Clin Pharmacol. 2001;41:1301–1309. [PubMed] [Google Scholar]
47. Fujimura A, Sasaki M, Harada K, et al. Influences of bathing and hot weather on the pharmacokinetics of a new transdermal clonidine, M-5041T. J Clin Pharmacol. 1996;36:892–896. [PubMed] [Google Scholar]
48. Archer DF, Stanczyk FZ, Rubin A, et al. Pharmacokinetics and adhesion of the Agile transdermal contraceptive patch (AG200-15) during daily exposure to external conditions of heat, humidity and exercise. Contraception. 2013;87:212–219. doi: 10.1016/j.contraception.2012.10.009. [PubMed] [CrossRef] [Google Scholar]
49. Ashburn MA, Ogden LL, Zhang J, et al. The pharmacokinetics of transdermal fentanyl delivered with and without controlled heat. J Pain. 2003;4:291–297. [PubMed] [Google Scholar]
50. Gjesdal K, Klemsdal TO, Rykke EO, et al. Transdermal nitrate therapy: bioavailability during exercise increases transiently after the daily change of patch. Br J Clin Pharmacol. 1991;31:560–562. [PMC free article] [PubMed] [Google Scholar]
51. Vanakoski J, Seppälä T, Sievi E, et al. Exposure to high ambient temperature increases absorption and plasma concentrations of transdermal nicotine. Clin Pharmacol Ther. 1996;60:308–315. doi: 10.1016/S0009-9236(96)90057-0. [PubMed] [CrossRef] [Google Scholar]
52. Bur A, Joukhadar C, Klein N, et al. Effect of exercise on transdermal nicotine release in healthy habitual smokers. Int J Clin Pharmacol Ther. 2005;43:239–243. [PubMed] [Google Scholar]
53. Klemsdal TO, Gjesdal K, Zahlsen K. Physical exercise increases plasma concentrations of nicotine during treatment with a nicotine patch. Br J Clin Pharmacol. 1995;39:677–679. [PMC free article] [PubMed] [Google Scholar]
54. Marriott TB, Charney MR, Stanworth S. Effects of application durations and heat on the pharmacokinetic properties of drug delivered by a lidocaine/tetracaine patch: a randomized, open-label, controlled study in healthy volunteers. Clin Ther. 2012;34:2174–2183. doi: 10.1016/j.clinthera.2012.08.008. [PubMed] [CrossRef] [Google Scholar]
55. Danon A, Ben-Shimon S, Ben-Zvi Z. Effect of exercise and heat exposure on percutaneous absorption of methyl salicylate. Eur J Clin Pharmacol. 1986;31:49–52. [PubMed] [Google Scholar]
56. Mizushima H, Inoue K, Ishizuka H. The effects of external heating on the permeation of oxybutynin through human epidermal membrane. Biol Pharm Bull. 2007;30:612–615. [PubMed] [Google Scholar]
57•. Prodduturi S, Sadrieh N, Wokovich AM, et al. Transdermal delivery of fentanyl from matrix and reservoir systems: effect of heat and compromised skin. J Pharm Sci. 2010;99:2357–66. doi: 10.1002/jps.22004. This paper investigated heat effect on fentanyl release from two transdermal delivery systems with different TDS designs and skin permeation in vitro. [PubMed] [CrossRef] [Google Scholar]
58. Curry SE, Finkel JC. Use of the Synera patch for local anesthesia before vascular access procedures: a randomized, double-blind, placebo-controlled study. Pain Med. 2007;8:497–502. doi: 10.1111/j.1526-4637.2006.00204.x. [PubMed] [CrossRef] [Google Scholar]
59. Franz TJ, Lehman PA, Raney SG. Use of excised human skin to assess the bioequivalence of topical products. Skin Pharmacol Physiol. 2009;22:276–286. doi: 10.1159/000235828. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
60. Lehman PA, Raney SG, Franz TJ. Percutaneous absorption in man: in vitro-in vivo correlation. Skin Pharmacol Physiol. 2011;24:224–230. doi: 10.1159/000324884. [PubMed] [CrossRef] [Google Scholar]
Formats:
Article | PubReader | ePub (beta) | PDF (118K) | Cite
Share
Share on Facebook FacebookShare on Twitter TwitterShare on Google Plus Google+
Save items
View more options
Similar articles in PubMed
On the Road to Development of an in Vitro Permeation Test (IVPT) Model to Compare Heat Effects on Transdermal Delivery Systems: Exploratory Studies with Nicotine and Fentanyl.
[Pharm Res. 2017]
Future of the transdermal drug delivery market--have we barely touched the surface?
[Expert Opin Drug Deliv. 2016]
Evaluation of Heat Effects on Transdermal Nicotine Delivery In Vitro and In Silico Using Heat-Enhanced Transport Model Analysis.
[AAPS J. 2020]
Application of methyl methacrylate copolymers to the development of transdermal or loco-regional drug delivery systems.
[Expert Opin Drug Deliv. 2014]
In vitro-in vivo correlations for nicotine transdermal delivery systems evaluated by both in vitro skin permeation (IVPT) and in vivo serum pharmacokinetics under the influence of transient heat application.
[J Control Release. 2018]
See reviews...
See all...
Cited by other articles in PMC
Pharmacokinetic Profile of Fentanyl in the Koala (Phascolarctos cinereus) after Intravenous Administration, and Absorption via a Transdermal Patch
[Animals : an Open Access Journ...]
Remote Temperature-Responsive Parafilm Dermal Patch for On-Demand Topical Drug Delivery
[Micromachines. 2021]
Pharmacokinetic Profile of the Asenapine Transdermal System (HP-3070)
[Journal of Clinical Psychophar...]
Enhancing Permeation of Drug Molecules Across the Skin via Delivery in Nanocarriers: Novel Strategies for Effective Transdermal Applications
[Frontiers in Bioengineering an...]
Development of Skin-On-A-Chip Platforms for Different Utilizations: Factors to Be Considered
[Micromachines. 2021]
See all...
Links
MedGen
PubMed
Taxonomy
Recent Activity
ClearTurn Off
Heat effects on drug delivery across human skin
Heat effects on drug delivery across human skin
NIHPA Author Manuscripts. 2016 May; 13(5)755
See more...
Heat-related toxicity with the fentanyl transdermal patch.
[J Pain Symptom Manage. 1998]
Heat-associated increase in transdermal fentanyl absorption.
[Am J Health Syst Pharm. 2003]
Studies of Thermal Injury: I. The Conduction of Heat to and through Skin and the Temperatures Attained Therein. A Theoretical and an Experimental Investigation.
[Am J Pathol. 1947]
Review Human thermoregulation and measurement of body temperature in exercise and clinical settings.
[Ann Acad Med Singap. 2008]
Review Skin blood flow in adult human thermoregulation: how it works, when it does not, and why.
[Mayo Clin Proc. 2003]
Role of sympathetic nerves in the vascular effects of local temperature in human forearm skin.
[Am J Physiol. 1993]
Cutaneous vasomotor reactions in response to controlled heat applied on various body regions of healthy humans: evaluation of time course and application parameters.
[Int J Physiol Pathophysiol Pharmacol. 2011]
Understanding heat facilitated drug transport across human epidermis.
[Eur J Pharm Biopharm. 2012]
Effect of local controlled heat on transdermal delivery of nicotine.
[Int J Physiol Pathophysiol Pharmacol. 2011]
Role of nitric oxide in the vascular effects of local warming of the skin in humans.
[J Appl Physiol (1985). 1999]
Review Skin blood flow in adult human thermoregulation: how it works, when it does not, and why.
[Mayo Clin Proc. 2003]
The influence of topical capsaicin on the local thermal control of skin blood flow in humans.
[Am J Physiol Regul Integr Comp Physiol. 2001]
Role of sympathetic nerves in the vascular effects of local temperature in human forearm skin.
[Am J Physiol. 1993]
See more ...
The effect of temperature on blood flow and deep temperature in the human forearm.
[J Physiol. 1943]
Effect of high local temperature on reflex cutaneous vasodilation.
[J Appl Physiol Respir Environ Exerc Physiol. 1984]
See more ...
Thermoregulation during rest and exercise in different postures in a hot humid environment.
[J Appl Physiol Respir Environ Exerc Physiol. 1980]
Human thermoregulation in sauna.
[Ann Clin Res. 1988]
Assessing the impact of heat on the systemic delivery of fentanyl through the transdermal fentanyl delivery system.
[Pain Med. 2000]
A pilot study assessing the impact of heat on the transdermal delivery of testosterone.
[J Clin Pharmacol. 2001]
Thermoregulation during rest and exercise in different postures in a hot humid environment.
[J Appl Physiol Respir Environ Exerc Physiol. 1980]
See more ...
Review Human thermoregulation and measurement of body temperature in exercise and clinical settings.
[Ann Acad Med Singap. 2008]
Review Skin blood flow in adult human thermoregulation: how it works, when it does not, and why.
[Mayo Clin Proc. 2003]
Effect of local controlled heat on transdermal delivery of nicotine.
[Int J Physiol Pathophysiol Pharmacol. 2011]
Effect of heat on the percutaneous absorption and skin retention of three model penetrants.
[Eur J Pharm Sci. 2004]
Understanding heat facilitated drug transport across human epidermis.
[Eur J Pharm Biopharm. 2012]
The effect of heat on skin permeability.
[Int J Pharm. 2008]
See more ...
Transdermal penetration of vasoconstrictors--present understanding and assessment of the human epidermal flux and retention of free bases and ion-pairs.
[Pharm Res. 2003]
Enhancement of topical delivery of drugs via direct penetration by reducing blood flow rate in skin.
[Int J Pharm. 2005]
Effects of vasoconstriction on dermal pharmacokinetics and local tissue distribution of compounds.
[J Pharm Sci. 1994]
Increased uptake of transdermal glyceryl trinitrate during physical exercise and during high ambient temperature.
[Am Heart J. 1986]
Heating and cooling of the nitroglycerin patch application area modify the plasma level of nitroglycerin.
[Eur J Clin Pharmacol. 1992]
Effect of local controlled heat on transdermal delivery of nicotine.
[Int J Physiol Pathophysiol Pharmacol. 2011]
Pressure-sensitive adhesives for transdermal drug delivery systems.
[Pharm Sci Technol Today. 1999]
Analysis of permeability data for the case of parallel diffusion pathways.
[Biophys J. 1966]
Mechanism of percutaneous absorption. 3. The effect of temperature on the transport of non-electrolytes across the skin.
[J Invest Dermatol. 1967]
The effect of temperature upon the permeation of polar and ionic solutes through human epidermal membrane.
[J Pharm Sci. 1995]
Understanding heat facilitated drug transport across human epidermis.
[Eur J Pharm Biopharm. 2012]
Temperature dependence of skin permeability to hydrophilic and hydrophobic solutes.
[J Pharm Sci. 2007]
Effect of heat on the percutaneous absorption and skin retention of three model penetrants.
[Eur J Pharm Sci. 2004]
Pharmacokinetics of norelgestromin and ethinyl estradiol delivered by a contraceptive patch (Ortho Evra/Evra) under conditions of heat, humidity, and exercise.
[J Clin Pharmacol. 2001]
Assessing the impact of heat on the systemic delivery of fentanyl through the transdermal fentanyl delivery system.
[Pain Med. 2000]
The pharmacokinetics of transdermal fentanyl delivered with and without controlled heat.
[J Pain. 2003]
Randomized 5-treatment crossover study to assess the effects of external heat on serum fentanyl concentrations during treatment with transdermal fentanyl systems.
[J Clin Pharmacol. 2012]
Effect of exercise and heat exposure on percutaneous absorption of methyl salicylate.
[Eur J Clin Pharmacol. 1986]
The experimental evaluation and molecular dynamics simulation of a heat-enhanced transdermal delivery system.
[AAPS PharmSciTech. 2013]
The effects of external heating on the permeation of oxybutynin through human epidermal membrane.
[Biol Pharm Bull. 2007]
Understanding heat facilitated drug transport across human epidermis.
[Eur J Pharm Biopharm. 2012]
Transdermal delivery of fentanyl from matrix and reservoir systems: effect of heat and compromised skin.
[J Pharm Sci. 2010]
Use of the Synera patch for local anesthesia before vascular access procedures: a randomized, double-blind, placebo-controlled study.
[Pain Med. 2007]
Effects of application durations and heat on the pharmacokinetic properties of drug delivered by a lidocaine/tetracaine patch: a randomized, open-label, controlled study in healthy volunteers.
[Clin Ther. 2012]
Increased uptake of transdermal glyceryl trinitrate during physical exercise and during high ambient temperature.
[Am Heart J. 1986]
Randomized 5-treatment crossover study to assess the effects of external heat on serum fentanyl concentrations during treatment with transdermal fentanyl systems.
[J Clin Pharmacol. 2012]
Heating and cooling of the nitroglycerin patch application area modify the plasma level of nitroglycerin.
[Eur J Clin Pharmacol. 1992]
Pharmacokinetics of norelgestromin and ethinyl estradiol delivered by a contraceptive patch (Ortho Evra/Evra) under conditions of heat, humidity, and exercise.
[J Clin Pharmacol. 2001]
Exposure to high ambient temperature increases absorption and plasma concentrations of transdermal nicotine.
[Clin Pharmacol Ther. 1996]
Use of excised human skin to assess the bioequivalence of topical products.
[Skin Pharmacol Physiol. 2009]
Percutaneous absorption in man: in vitro-in vivo correlation.
[Skin Pharmacol Physiol. 2011]
Effect of local controlled heat on transdermal delivery of nicotine.
[Int J Physiol Pathophysiol Pharmacol. 2011]
Increased uptake of transdermal glyceryl trinitrate during physical exercise and during high ambient temperature.
[Am Heart J. 1986]
Heating and cooling of the nitroglycerin patch application area modify the plasma level of nitroglycerin.
[Eur J Clin Pharmacol. 1992]
Support CenterSupport Center
Simple NCBI Directory
GETTING STARTED
NCBI Education
NCBI Help Manual
NCBI Handbook
Training & Tutorials
Submit Data
RESOURCES
Chemicals & Bioassays
Data & Software
DNA & RNA
Domains & Structures
Genes & Expression
Genetics & Medicine
Genomes & Maps
Homology
Literature
Proteins
Sequence Analysis
Taxonomy
Variation
POPULAR
PubMed
Bookshelf
PubMed Central
BLAST
Nucleotide
Genome
SNP
Gene
Protein
PubChem
FEATURED
Genetic Testing Registry
GenBank
Reference Sequences
Gene Expression Omnibus
Genome Data Viewer
Human Genome
Mouse Genome
Influenza Virus
Primer-BLAST
Sequence Read Archive
NCBI INFORMATION
About NCBI
Research at NCBI
NCBI News & Blog
NCBI FTP Site
NCBI on Facebook
NCBI on Twitter
NCBI on YouTube
Privacy Policy
External link. Please review our privacy policy.
NLMNIHDHHSUSA.gov
National Center for Biotechnology Information, U.S. National Library of Medicine
8600 Rockville Pike, Bethesda MD, 20894 USA
Policies and Guidelines | Contact
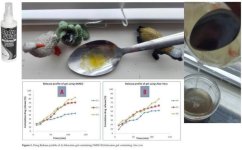 zzz+transdermal+pics.JPG51.7 KB · Views: 0
zzz+transdermal+pics.JPG51.7 KB · Views: 0 zzz+transdermal%2C+sublingual+pics+0.JPG45 KB · Views: 0
zzz+transdermal%2C+sublingual+pics+0.JPG45 KB · Views: 0